By Ann Neumann
“The Patient Body” is a monthly column about issues at the intersection of religion and medicine. You can read the October column here.
For the body is not one member, but many. –1 Corinthians 12:14, KJV
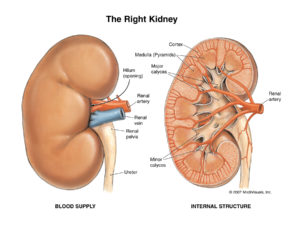
If I pay you $10,000, will you give me a kidney? Just one. You have two and you really only need one; you’re healthy, and while I don’t know you, I think you might have an idea of what to do with an extra ten G. I’ll cover your hospital stay, your operation, your recovery*, all you have to do is… let my surgeon cut into your abdomen and take your kidney. You’ll be saving a life. You’ll be richer. You’ll be giving the ultimate gift.
This is about the same deal that Raymond Crockett, a London doctor, struck with four Turks in 1989: cash for kidneys (he paid each about $6,000). The medical world was rocked when it discovered what Crockett was doing. And from, of all places, his office on London’s Harley Street, an address that since the 1800s has been synonymous with well-respected medical practice. The organ trade had slapped the medical community on its most ethical flank. They and the global media were aghast.
Immediately the UK passed the Human Organ Transplants Act, imposing fines and censure on doctors who participated in fee-for-organ transplants. The World Health Assembly convened in 2004 to stop such trade; the meeting resulted in the passage of The Declaration of Istanbul in 2008, the preamble of which in part reads:
Organ transplantation, one of the medical miracles of the twentieth century, has prolonged and improved the lives of hundreds of thousands of patients worldwide. The many great scientific and clinical advances of dedicated health professionals, as well as countless acts of generosity by organ donors and their families, have made transplantation not only a life-saving therapy but a shining symbol of human solidarity. Yet these accomplishments have been tarnished by numerous reports of trafficking in human beings who are used as sources of organs and of patient-tourists from rich countries who travel abroad to purchase organs from poor people.
On its surface, a “black market” trade of organs is repulsive, its censure obvious. And yet, as doctors, philosophers and bioethicists have asked since the Harley Street incident, what motivates our visceral reaction to payment for organ donation? Our assumption that the most poor will be coerced by money? Our belief that (parts of) the human body should not be commodified? Our hope that “human solidarity” is preserved in the altruistic gift of organs–by the living and dead–because donation saves the lives of others?
As far as organ donation goes, “human solidarity” isn’t working. As I write, there are more than 105,000 patients in the US waiting for a kidney. Each year, the waiting list increases by three to four thousand.** A host of social and medical factors contribute to this exponential increase in the need for kidneys, including the aging US population, poor health and prevention (the two leading causes of end stage kidney disease, ESKD, are diabetes and high blood pressure), and a too-limited supply of viable kidney donations. Unlike other organs, kidneys can be “harvested” from living donors; other organs, like hearts and livers, cannot be removed until a patient is dead (And must be removed quickly! Organs degrade rapidly once they cease to receive oxygen via the blood).
This growing need for viable kidneys has increased pressure on the medical community to find new sources. Over the past twenty-five years, since transplantation became widely accessible, various studies have examined our resistance to a fee-for-kidney structure. One such study, conducted in 2010 by University of Pennsylvania’s Scott Halpern, found that those with an annual income of $20,000 a year were no more likely to donate a kidney than those making $100,000.
The study is provocative because it pinpoints one aspect of our revulsion to fee-for-kidney donations: it asks if financial incentive essentially results in coercion of the poor. In other words, are poor people more likely to donate a kidney if they are paid for it?
Because the conversation surrounding organ donation is a global one, the premise for concern is that kidneys will come from the poor who would most benefit from (or be susceptible to) payment, and that recipients will be the financially well-off. “The poor” in this case are primarily the global poor, people in “developing” countries for whom $10,000 might be worth more than an in-tact body. The Harley Street incident, one could say, supports this assumption. Yet, this scenario does not consider forms of regulation, at the state or international level, that could address transplant tourism, predatory middle men, or killing for organs. Too, it posits that those with empty pockets–regardless of what country they live in–place less value on their health or bodies, that they are vulnerable to wads of cash, that their vulnerability will override any sense of self-preservation or sound judgement they may have. Despite the Western world’s concern, naysayers counter, even the global poor have a right to decide what they do with their bodies, thank you very much.
What, then, is the cost of our prohibition on the sale of kidneys? A conference at Princeton University in October, “The Ethics of Transplants: Is Careless Thought Costing Lives?,” titled after a new book by Janet Radcliffe Richards, Professor of Practical Ethics at Oxford University, probed this question. The conference was coordinated by Frances Kissling, president of The Center for Health, Ethics and Social Policy and the former president of Catholics for Choice, and Peter Singer, a philosopher and Professor of Bioethics at Princeton.
In her keynote address, Richards wondered if perhaps our initial reaction to organ trade was caused by something other than our ethics, say, by our moral confusion. After all, how can it be legal to donate an organ if you know where it’s going (for instance, to a family member), but illegal to do so if you don’t? And what’s the matter with appropriate compensation when we have already compromised the no-fee policy for other body parts or products? One of the Harley Street Turks wanted the money to care for his ill child. The real question, Richards surmised, is about the legal status of donors.
Conference attendees cited examples of when we allow humans to sacrifice their bodies: women who act as child surrogates or carry pregnancies to term for the sake of adoption; soldiers sent off to war; routine payment for eggs for invitro fertilization. Others pragmatically noted the literal price paid by US society for all those missing kidneys, significantly, $34 billion spent a year on dialysis, a taxing process whereby a person can have excess toxins and water removed from their blood each week. It’s a privilege to think that discussing the cost of a kidney is crass, as any ill person will tell you. How many other ways, then, could $34 billion be used by our health care system to save lives? Still others noted that bodily autonomy, a principle of medical ethics, grants all patients control of their medical decisions–even when those decisions mean certain death.
In October, a team of Canadian researchers published a new study in the Clinical Journal of the American Society of Nephrology that sought the optimal price for a kidney. $10,000, they found, was about right in the US market. In an article at NBCNews Health, Arthur Caplan, a bioethicist at New York University’s Langone Medical Center, writes that even though 40% of Americans polled said they might be willing to donate a kidney for the right price, there is “no guarantee that more kidneys will become available or that harm will not be done to the rest of the organ transplant system.” Telling a researcher you’d give up a kidney is one thing, crawling onto the operating table and under the knife is another. If kidneys in America bring $10,000, what would the price be for a heart? A lung? And how do you prevent killing for organs?
Caplan notes another deterrent to donation: religion. “Several religions–including Catholicism, many conservative Protestant sects and others–strongly oppose any form of organ sales. Their theology says that you do not own your body, it is a gift from God, so it is not something you can choose to sell.” Pope Benedict, Caplan notes, forbid the buying and selling of organs. We all know that believers don’t always do what their leaders, priests and pope tell them to (think of the 98% of Catholic women using contraception). Caplan’s point is that paying for kidneys may still not achieve a 5% increase in donations… and religious belief is just one more deterrent. Five percent doesn’t put a dent in the 105,000 US citizens who are already waiting.
But there’s another point to be made from Caplan’s mention of religion. With the Catholic Church managing about 650 hospitals in the US and playing such a strong role in the formation of health care policy, what would the Vatican say about paid-for kidneys? Most certainly, the one-fifth of all US hospital beds they manage wouldn’t be used for paid donation.
How then, across cultures, classes, religions, borders and currencies, do we find an ethical solution to the kidney shortage? What would a fair, compassionate and just kidney trade look like? And how do you regulate it, both nationally and internationally? Here, in the nuts-and-bolts formation of health care policy–and not in a back office on Harley Street–is where “moral confusion” meets a “gift from God.”
*The long-term risks of kidney donation may vary.
**About 30% of patients on the kidney waiting list are considered “inactive” because they are not healthy enough for a transplant, either because of their medical status or because they are still being prepared for transplant. See here for more details. About 4,400 people die waiting for kidneys each year, although this number is perhaps misleading. Not all kidney recipients return to perfect health; not all those hoping for a transplant are otherwise healthy.
Ann Neumann is a Visiting Scholar at the Center for Religion and Media at New York University and contributing editor at The Revealer where she writes the column “The Patient Body.” She’s written for Guernica magazine, New York Law Review (forthcoming, January 2014), Religion & Politics, Killing the Buddha, and The Nation, among others. Her chapter on class and hospice use will appear in Living with Class: Philosophical Reflections on Identity and Material Culture (Palgrave Macmillan, December 2013), edited by Brian Seitz and Ron Scapp. Neumann is currently writing a book about a good death.