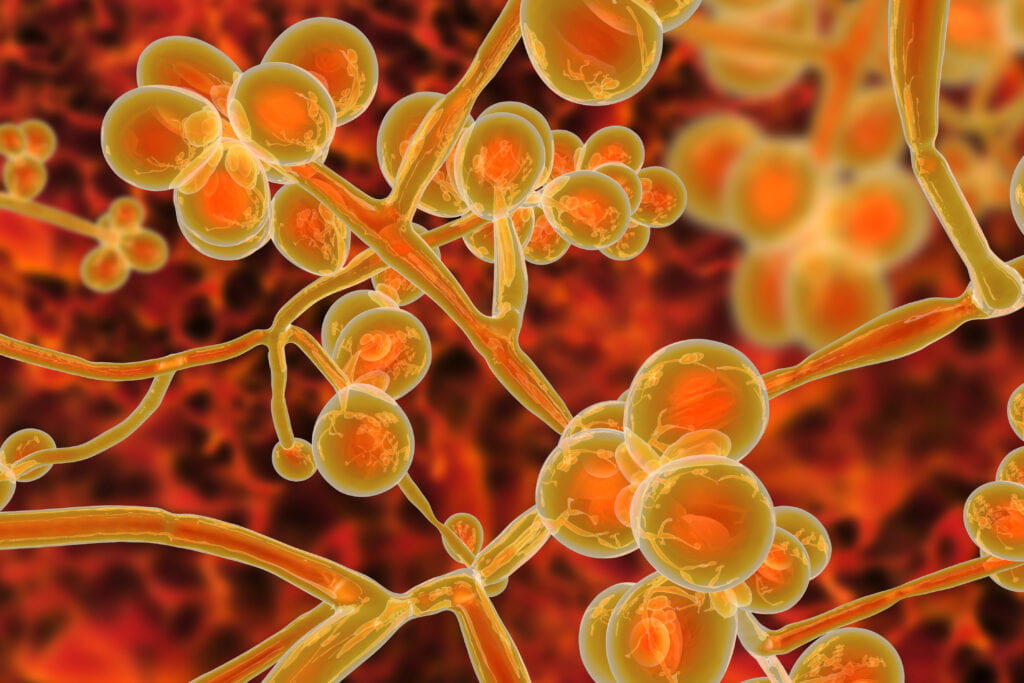
Candida Auris is a very dangerous, drug-resistant, hospital-acquired fungal infection that has been detected in 600 cases in the United States. Yu uses the experience of Stephanie Spoor in 2019 to describe the clinical history and public health outcomes.
Stephanie, who was aged 64 at the time, was undergoing Lupus treatment and had a vulnerable immune system. This allowed the fungus to enter her bloodstream through a contaminated catheter and evade her weakened immune response. Immediately after diagnosis, the treating team arranged for Ms. Spoor to be isolated from the rest of the patient population in an attempt to limit the spread of the C. auris infection, Yu reports. As the patient’s health continued to deteriorate, the treating team used an extracorporeal membrane oxygenation machine to help with breathing, but it proved to be of little success.
Yu alludes that the strict infection control measures implemented were successful at curbing the spread of the fungus. Fast screening tests were utilized to detect the fungus early on, use of specialized disinfection equipment and solutions, and replacing contaminated items were strategies Yu considers to have had a likely positive impact.
Heather attributes the lack of transparency between healthcare facilities and the public is due to fear of public backlash but emphasizes the necessity of efficient communication to protect patients and increase awareness of hospital-acquired infections.
