Development of Pediatric Orthoses using Atypical Materials: Description and need of product
My competence project product involved learning how to make custom orthoses from less commonly used materials. Oftentimes, prefabricated splints and even custom orthoses from conventional materials like low temperature thermoplastics, usually used for orthosis fabrication, do not work for the pediatric population. I used my competence project to advance my knowledge about fabrication materials and techniques. I further tried them with my pediatric/adolescent clients for real world experience.
This first case product scenario, addressed client-specific functional goals to improve the quality of task completions. The needs of this client were addressed using both aluminum wire and neoprene products. By addressing the client’s aesthetic needs, cultural needs, and social environmental needs, the atypical products were successfully integrated into the client’s lifestyle. Thereby improving compliance and increased wearing time which maximized the outcomes.
THEORETICAL BASE: The biomechanical and occupational adaptation frames of references were used.
Literature Review Highlights: This portion was also in my professional presentation to OT colleagues.
LITERATURE REVIEW HIGHLIGHTS
A literature search revealed no articles that studied the use of aluminum wire orthoses versus neoprene orthoses as compared to thermoplastics. However, the use of custom orthoses, despite the material used, has been shown to be effective. The main takeaway is that the orthosis will work if the client chooses to wear it. Thus, it is up to the therapist to use knowledge of occupational adaptation frames of reference to adapt the custom orthosis for the client to increase compliance wear.
The following brief synopsis of articles demonstrates support for orthoses with various purposes, using various materials with children:
Koh et al. (2012) performed a level III retrospective comparative study of the use of orthoses for children with trigger thumb or locked thumb IP joints and concluded that orthosis wear was efficient in shortening the time for symptoms relief. For pediatric hand spasticity, intermittent static casting of the wrist demonstrated improvements in range of motion, quality of movements, and functional use of the hand (Wilton 2003). In these cases, Hepworth (2017) determined that most therapists’ preferences for material were a combination of thermoplastic and neoprene (57.5%), neoprene (27.4%), thermoplastic (5.0%). Thumb abduction splinting has been found to improve hand function in children with cerebral palsy who have thumb-in-palm deformity (Dorich & Shotwell, 2014; Hughes, Franzsen & Freeme, 2017). A child with substantial ligamentous laxity and chronic wrist pain who consistently has pain with writing and poor CMC joint stability may experience less pain when using a neoprene wrist and thumb spica orthotic (Dorich & Shotwell, 2014). The compression provided by neoprene material may also assist in scar management. Yelvington et al. (2013) found a statistically significant reduction in hypertrophic scars.
CASE PRODUCT SCENARIO
Client Characteristics: J.F. is a 17 y.o. female who was born with Erb’s Palsy. J.F. presented to OT s/p right biceps rerouting procedure to facilitate elbow flexion and neutral wrist extension. The OT evaluation revealed that J.F. was unsure how to use her right arm in bi-manual activities. J.F immediately identified improving typing skills for eventual college admission into optometry school. J.F.’s mother was concerned about increasing independence in ADL’s when J.F. goes to college which included being independent in buttoning skills. J. F. also suggested strengthening her arm to participate in gym class. J.F.’s most meaningful goal was to inhibit “the fingers curling in”, as in inhibiting flexor tone, during plank exercises.
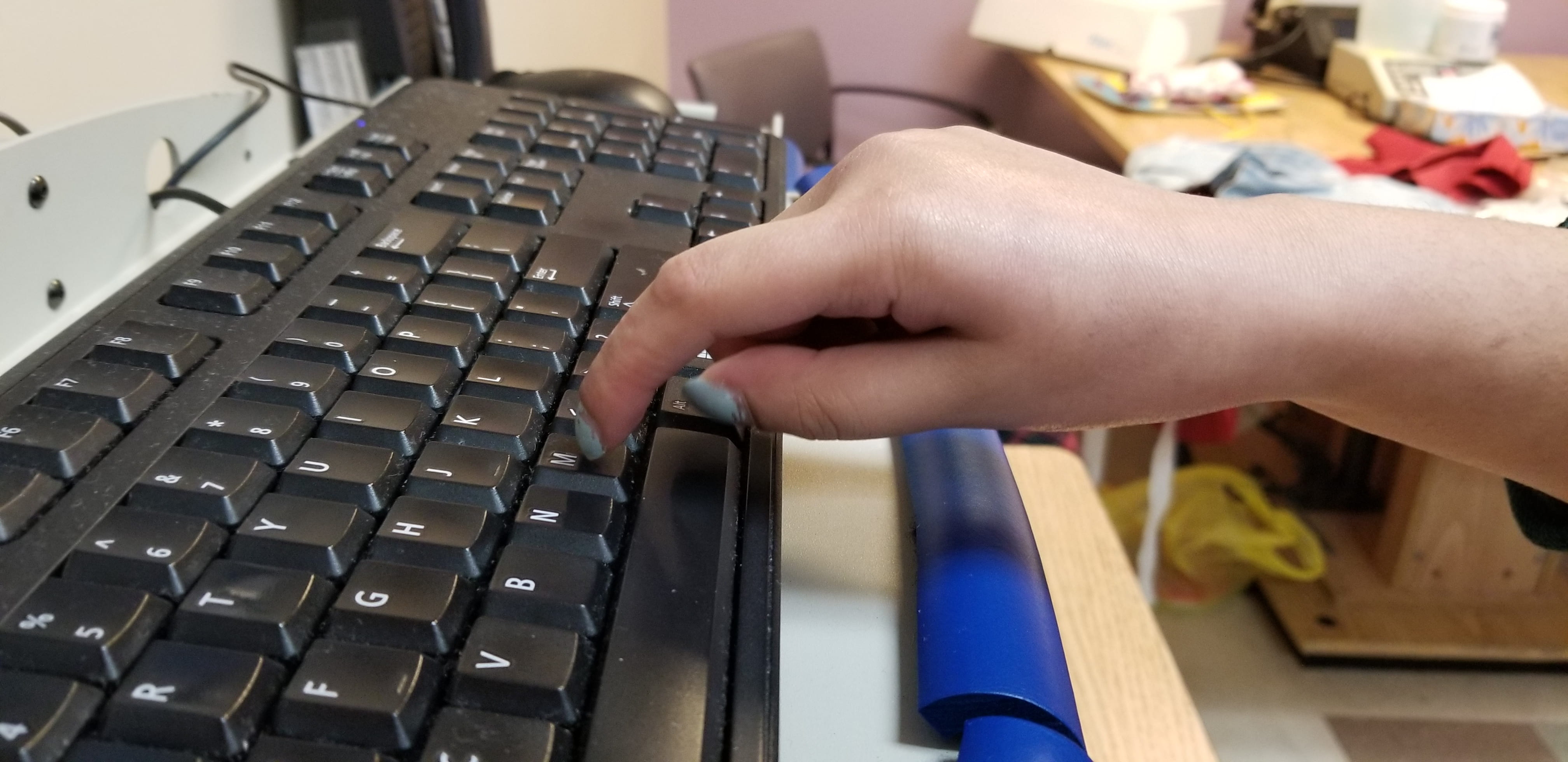
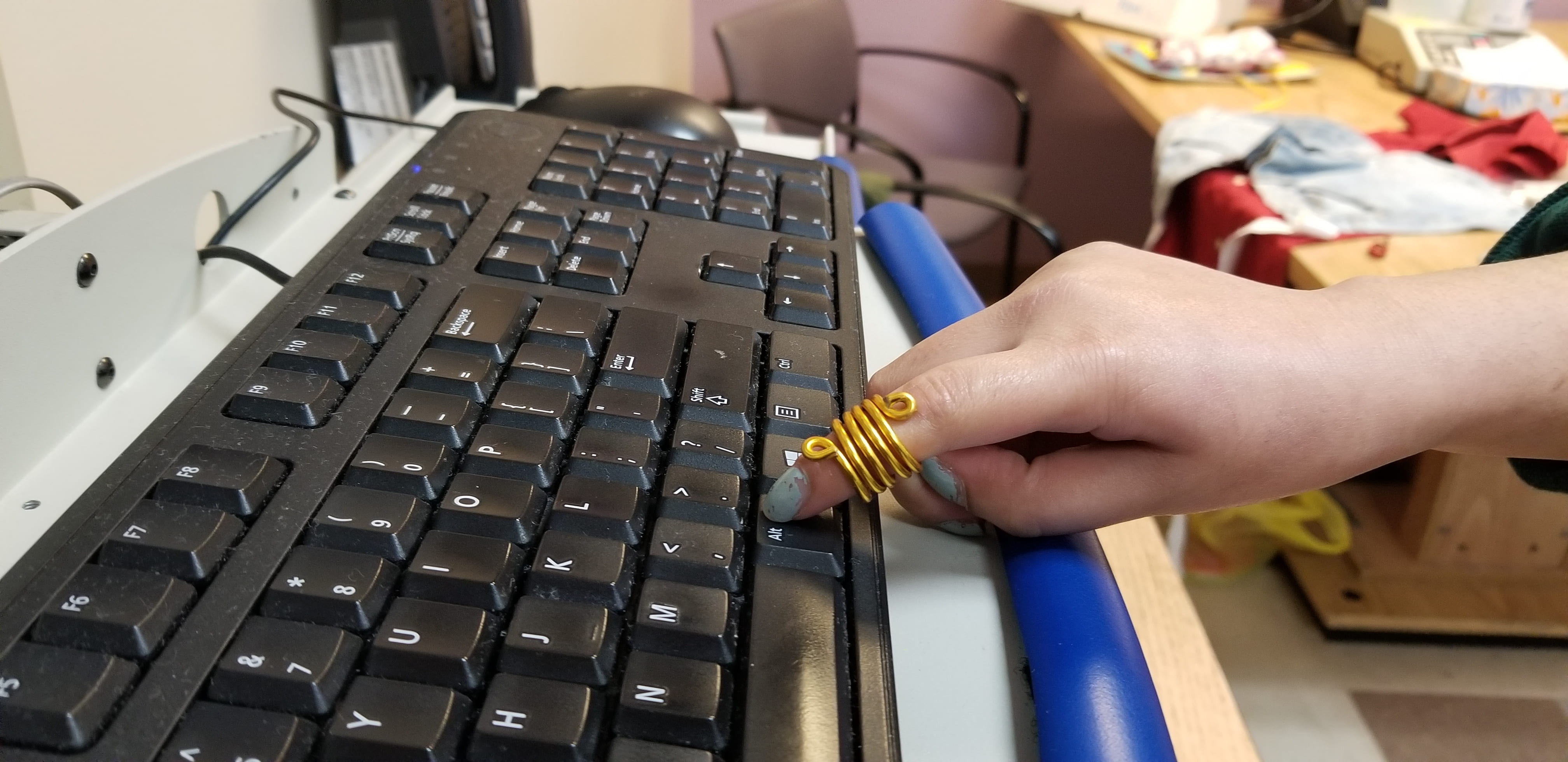
- Improving Typing Skills (custom Aluminum Wire Orthosis)
2. Improving ADL’s: Buttoning Skills (custom Aluminum Wire Orthosis)


3. Improving positioning in order to perform a Plank position in gym class (custom Neoprene Glove)
Before and after with custom neoprene glove and orficast inserts. No more interference from tone as digits are in extended position and J.F. can weight-bear comfortably.
(see below how the neoprene glove product was designed and adapted in stages as per client feedback)
Assessments used to measure outcomes
| Table 1
This is a table comparing the wear times of traditional versus atypical orthosis materials by client J.F.. |
||
| WEAR TIME | ||
| Traditional Orthosis Material | Custom Thermoplastic Oval-8 | Worn intermittently at home |
| Atypical Orthosis Material | Custom Aluminum Wire Orthosis | Worn every day during typing at school and worn at school for buttoning, when changing clothes between gym classes |
| Traditional Orthosis Material | Custom Thermoplastic Paddle Orthosis | Worn only at night |
| Atypical Orthosis Material | Custom Neoprene Glove | Worn every week for gym class |
| Table 2
This is a table demonstrating the results of the outcome measures at initial evaluation and at discharge, after J.F. utilized the atypical materials for a period of three months. This is consistent with the biomechanical frame of reference
|
|||||
| Patient-Specific Functional Scale (PSFS) | Moberg Pickup Test
(eyes open) |
Hand grip/pinch Strength | Numerical Rating Scale for pain | Right Hand composite ROM in degrees | |
| Initial evaluation | 3/50 | Picked up 5 out of 12 thick items in 1 min | Grip: 5.8 lbs
Lateral Pinch: 1 lb |
3/10 | MCP 40-85
PIP 45-80 DIP 10-50 |
| Discharge | 30/50 | Picked up 11 out of 12 items in 3 mins | Grip: 21.4 lbs
Lateral Pinch: 6 lbs |
0/10 | MCP same
PIP 35-100 DIP 5-55 |
The above five assessments were selected to demonstrate the outcomes of using the atypical products for this case. Grip/pinch assessments using the hand-held dynamometer and pinch meter are standardized assessments that have evidenced-based norms, reliability and validity for use not only in adult populations, but also in pediatrics and adolescents. Reference: Mathiowetz, V., Wiemer, D. M., & Federman, S. M. (1986). Grip and pinch strength: Norms for 6- to 19-year-olds. The American Journal of Occupational Therapy. : Official Publication of the American Occupational Therapy Association, 40(10), 705–711. https://doi-org.proxy.library.nyu.edu/10.5014/ajot.40.10.705.
The other three assessments, as described below, were chosen because they also demonstrate reliability and validity.
-
-
- The PSFS was used as a quick functional goal attainment assessment where the patient determines how successful they are in their five chosen client-specific goals between a value of 0 to 10. Reference: Fairbairn, K., May, K., Yang, Y., Balasundar, S., Hefford, C., & Abbott, J. H. (2012). Mapping Patient-Specific Functional Scale (PSFS) items to the International Classification of Functioning, Disability and Health (ICF). Physical Therapy, 92(2), 310–317. https://doi-org.proxy.library.nyu.edu/10.2522/ptj.20090382
- The Moberg Pickup Test was used to assess hand dexterity. The standardized Moberg Pickup Test is reported to have a good to excellent test-retest and inter-rater reliability with a coefficient alpha for test-retest reliability of 0.985. Reference: Amirjani, N., Ashworth, N. L., Gordon, T., Edwards, D. C., & Chan, K. M. (2007). Normative values and the effects of age, gender, and handedness on the Moberg Pick-Up Test. MUSCLE & NERVE, 6, 788-792. https://doi-org.proxy.library.nyu.edu/10.1002/mus.20750
- The Numerical Rating Scale for pain was chosen because the client had no cognitive impairments which would affect her ability to accurately communicate her pain level on a scale of 0-10. The Numerical Rating Scale is considered to be valid and reliable for the adolescent population. Reference: Tsze, D. S., von Baeyer, C. L., Pahalyants, V., & Dayan, P. S. (2018). Validity and reliability of the verbal Numerical Rating Scale for children aged 4 to 17 Years with acute pain. Annals of Emergency Medicine, 71(6), 691–702. https://doi-org.proxy.library.nyu.edu/10.1016/j.annemergmed.2017.09.009
-
Therefore, the objectives were met for goal number one. I used the knowledge gained to expand my expertise in hand therapy and the effectiveness of the products was demonstrated. This is evidenced by the discharge numbers in the table above.
Neoprene Glove Product adapted as per client feedback (Consistent with occupational adaptation frame of reference)
Timeline to develop the products
Future directions/limitations/improvements
[Goal 2 ]


